
PDF Publication Title:
Text from PDF Page: 003
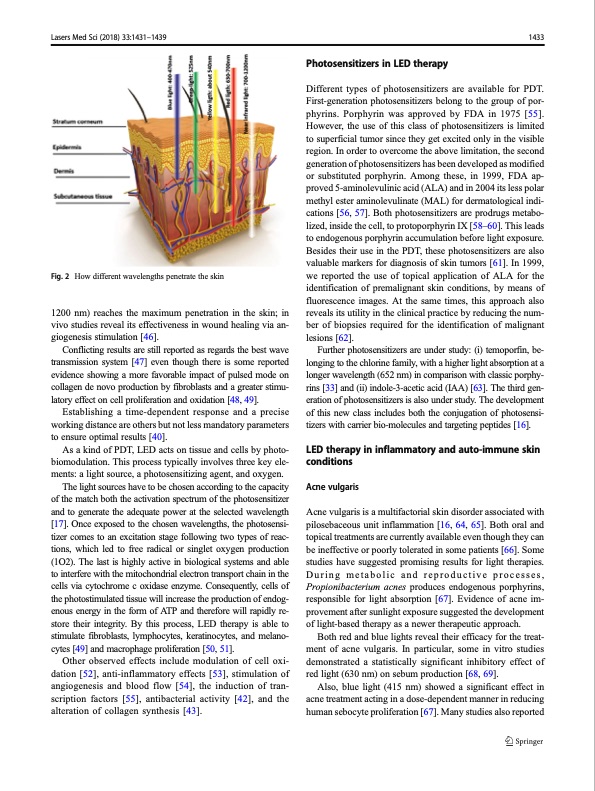
Lasers Med Sci (2018) 33:1431–1439 1433 Fig.2 Howdifferentwavelengthspenetratetheskin 1200 nm) reaches the maximum penetration in the skin; in vivo studies reveal its effectiveness in wound healing via an- giogenesis stimulation [46]. Conflicting results are still reported as regards the best wave transmission system [47] even though there is some reported evidence showing a more favorable impact of pulsed mode on collagen de novo production by fibroblasts and a greater stimu- latory effect on cell proliferation and oxidation [48, 49]. Establishing a time-dependent response and a precise working distance are others but not less mandatory parameters to ensure optimal results [40]. As a kind of PDT, LED acts on tissue and cells by photo- biomodulation. This process typically involves three key ele- ments: a light source, a photosensitizing agent, and oxygen. The light sources have to be chosen according to the capacity of the match both the activation spectrum of the photosensitizer and to generate the adequate power at the selected wavelength [17]. Once exposed to the chosen wavelengths, the photosensi- tizer comes to an excitation stage following two types of reac- tions, which led to free radical or singlet oxygen production (1O2). The last is highly active in biological systems and able to interfere with the mitochondrial electron transport chain in the cells via cytochrome c oxidase enzyme. Consequently, cells of the photostimulated tissue will increase the production of endog- enous energy in the form of ATP and therefore will rapidly re- store their integrity. By this process, LED therapy is able to stimulate fibroblasts, lymphocytes, keratinocytes, and melano- cytes [49] and macrophage proliferation [50, 51]. Other observed effects include modulation of cell oxi- dation [52], anti-inflammatory effects [53], stimulation of angiogenesis and blood flow [54], the induction of tran- scription factors [55], antibacterial activity [42], and the alteration of collagen synthesis [43]. Different types of photosensitizers are available for PDT. First-generation photosensitizers belong to the group of por- phyrins. Porphyrin was approved by FDA in 1975 [55]. However, the use of this class of photosensitizers is limited to superficial tumor since they get excited only in the visible region. In order to overcome the above limitation, the second generation of photosensitizers has been developed as modified or substituted porphyrin. Among these, in 1999, FDA ap- proved 5-aminolevulinic acid (ALA) and in 2004 its less polar methyl ester aminolevulinate (MAL) for dermatological indi- cations [56, 57]. Both photosensitizers are prodrugs metabo- lized, inside the cell, to protoporphyrin IX [58–60]. This leads to endogenous porphyrin accumulation before light exposure. Besides their use in the PDT, these photosensitizers are also valuable markers for diagnosis of skin tumors [61]. In 1999, we reported the use of topical application of ALA for the identification of premalignant skin conditions, by means of fluorescence images. At the same times, this approach also reveals its utility in the clinical practice by reducing the num- ber of biopsies required for the identification of malignant lesions [62]. Further photosensitizers are under study: (i) temoporfin, be- longing to the chlorine family, with a higher light absorption at a longer wavelength (652 nm) in comparison with classic porphy- rins [33] and (ii) indole-3-acetic acid (IAA) [63]. The third gen- eration of photosensitizers is also under study. The development of this new class includes both the conjugation of photosensi- tizers with carrier bio-molecules and targeting peptides [16]. LED therapy in inflammatory and auto-immune skin conditions Acne vulgaris Acne vulgaris is a multifactorial skin disorder associated with pilosebaceous unit inflammation [16, 64, 65]. Both oral and topical treatments are currently available even though they can be ineffective or poorly tolerated in some patients [66]. Some studies have suggested promising results for light therapies. During metabolic and reproductive processes, Propionibacterium acnes produces endogenous porphyrins, responsible for light absorption [67]. Evidence of acne im- provement after sunlight exposure suggested the development of light-based therapy as a newer therapeutic approach. Both red and blue lights reveal their efficacy for the treat- ment of acne vulgaris. In particular, some in vitro studies demonstrated a statistically significant inhibitory effect of red light (630 nm) on sebum production [68, 69]. Also, blue light (415 nm) showed a significant effect in acne treatment acting in a dose-dependent manner in reducing human sebocyte proliferation [67]. Many studies also reported Photosensitizers in LED therapyPDF Image | Photodynamic and photobiological effects of (LED) therapy
PDF Search Title:
Photodynamic and photobiological effects of (LED) therapyOriginal File Name Searched:
10103_2018_Article_2584.pdfDIY PDF Search: Google It | Yahoo | Bing
Cruise Ship Reviews | Luxury Resort | Jet | Yacht | and Travel Tech More Info
Cruising Review Topics and Articles More Info
Software based on Filemaker for the travel industry More Info
The Burgenstock Resort: Reviews on CruisingReview website... More Info
Resort Reviews: World Class resorts... More Info
The Riffelalp Resort: Reviews on CruisingReview website... More Info
| CONTACT TEL: 608-238-6001 Email: greg@cruisingreview.com | RSS | AMP |